Isle of Wight County residents are facing a significant loss of years of life before the age of 75, with an estimated 7,600 years lost per 100,000 individuals. This data was recently published by the University of Wisconsin’s Population Health Institute to provide insights into health outcomes at the county level, considering the diverse lifestyles and population densities across rural and urban areas.
Compared to national statistics, Isle of Wight, with a population of just over 40,000, is slightly below the state average but on par with the nation concerning premature deaths. Virginians who pass away before reaching 75 years old are forfeiting 7,300 years per 100,000 residents, while the national average stands at 8,000 years. In contrast, the sparsely populated Surry County, with 6,500 residents, is experiencing a higher rate of premature deaths, with 8,800 years lost per 100,000 individuals.
A breakdown of Isle of Wight’s 7,600 estimate reveals a concerning disparity in premature deaths between Black and white residents. The African American population in the county is losing a collective 12,000 years of life per 100,000 individuals, nearly double the 6,400 years lost by white residents. Black residents represent around 23% of the county’s total population.
Surry County, on the other hand, lacks specific data on the disaggregation by race in the latest reports. However, previous findings from 2021 indicated a similar trend, with 14,400 years lost per 100,000 for Black residents compared to 8,700 for white residents.
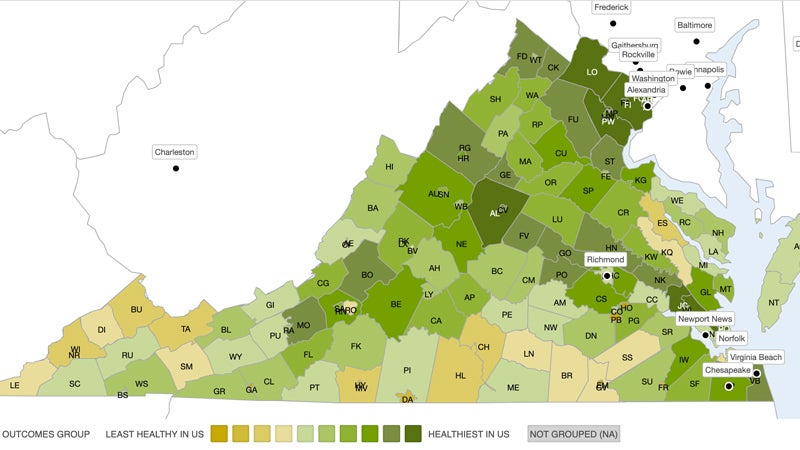
In terms of life expectancy, Isle of Wight averages 77.8 years, ranking 40th among Virginia’s 133 cities and counties, while Surry trails behind at 76.8 years, placing 52nd. The cities and counties in Northern Virginia boast the highest life expectancies, ranging from 82.5 to 85.3 years, while Franklin, bordering Isle of Wight to the south, is among the bottom five with a life expectancy of 67.9 years.
Cancer remains the leading cause of premature deaths in both Isle of Wight and Surry, followed by heart disease and accidents. COVID-19 emerged as the fourth leading cause in Isle of Wight, contributing to 41 under-75 deaths from 2019 to 2021. The lack of a disaggregation for Surry’s COVID-19-related deaths in the 2024 report highlights the ongoing challenges in addressing health disparities.
The report not only focuses on health outcomes but also delves into contributing factors such as access to medical care, poverty rates among children, and civic engagement indicators like voter turnout. It emphasizes the importance of well-resourced civic infrastructure in promoting better health outcomes and social and economic opportunities for communities.
Isle of Wight faces a shortage of primary care physicians and mental health practitioners compared to state averages, highlighting the need for improved healthcare access. The upcoming Riverside Smithfield Hospital, set to serve both Isle of Wight and Surry, aims to address some of these healthcare gaps upon its anticipated opening in early 2025.